Did you know over 50 million people in the US are affected by acne yearly? Among these, fungal acne and hormonal acne often cause confusion. These are two very different types of acne.
It’s important to know the differences between these acne types for effective treatment. Hormonal acne usually affects women during life stages like pregnancy. On the other hand, fungal acne is due to yeast overgrowth on the skin.
In this piece, we’ll dive into these skin conditions. You’ll learn how to spot their symptoms and understand treatment options. Knowing this info is your best tool against these skin issues!
Key Takeaways
- Acne’s causes vary, needing different treatments.
- Fungal acne, often mistaken for bacterial acne, needs antifungal treatment.
- Hormonal acne typically shows up on the jawline due to hormonal shifts.
- A steady skincare routine helps manage both acne types.
- A dermatologist’s guidance is key for correct diagnosis and treatment.
Introduction to Acne
Acne is a prevalent skin condition that affects people of all ages. It shows up as blackheads, whiteheads, and sometimes cysts. The problem starts when hair follicles get blocked by too much oil and inflammation.
Knowing the acne causes helps you choose the right skincare and treatments. Acne can happen because of hormone changes, especially in teens, or skin bacteria. Aware of this, you can spot acne symptoms and find good solutions.
Common factors influencing acne include:
- Excess oil production
- Clogged pores
- Inflammation
- Hormonal fluctuations
Understanding these causes offers a good skin condition overview. Knowing them can help you tackle acne more effectively. It leads to better skin care routines and healthier skin.
What is Fungal Acne?
Fungal acne is also known as Malassezia folliculitis. It’s different than the acne most people know. It comes from too much yeast growing in hair follicles. This can happen when it’s very humid or if you sweat a lot. If you see small, all-the-same-size bumps that itch, that might be fungal acne. It’s important to really understand what fungal acne is to treat it right.
Definition and Characteristics
Fungal acne shows up when yeast grows too much because of wet skin or oily products. You’ll see tiny, even bumps usually on your upper back, chest, or forehead. Regular acne treatments won’t work on these breakouts. In fact, they may even make things worse. There might also be red, swollen, and irritated skin that makes it hard to tell it apart from other kinds of acne.
Common Symptoms of Fungal Acne
People with fungal acne often notice certain signs. Here are some common fungal acne symptoms:
- Small, alike bumps mainly on the chest, upper back, and face.
- Itchy skin and irritation near the bumps.
- Feeling a sting after sweating a lot.
- Bumps that look like regular acne but feel different.
These symptoms make fungal acne tricky for people to understand how to treat it. That’s why seeing a dermatologist is key. They can figure out if it’s really fungal acne and find the best treatment. Some treatments that work for normal acne won’t work for fungal acne. It needs treatment that specifically targets yeast infections.
To learn more about how to manage hormonal acne and how hormones affect your skin, check out this helpful article.
Causes of Fungal Acne
To treat and prevent it well, knowing the fungal acne causes is key. Fungal acne, or pityrosporum folliculitis, happens mainly from too much Malassezia yeast on the skin. This imbalance triggers acne flare-ups, especially when the environment and certain habits change.
Overgrowth of Yeast (Malassezia)
The main issue with fungal acne is too much yeast. Usually, Malassezia is harmless on our skin. Yet, if it’s hot and you sweat a lot, the yeast grows too fast. This messes up the skin’s normal state and causes breakouts. Those with oily skin or weak immune systems are at most risk.
Triggering Factors
Many things can make skin yeast grow too much. Let’s look at a few:
- Staying in warm, wet places
- Wearing clothes that don’t let your skin breathe
- Not keeping clean
- Putting on oily skincare products
This makes the perfect place for yeast to grow and make symptoms worse. Knowing what causes flare-ups helps keep skin healthy. Stay clean and pick your skincare wisely. For more on fungal acne, see this article.

What is Hormonal Acne?
Hormonal acne is acne caused by changes in hormones. It’s common in women during key times like menstruation, pregnancy, and menopause. Knowing what hormonal acne is helps in treating it effectively.
Definition and Characteristics
Hormonal acne looks like deep, painful pimples and cysts mostly on the lower face. It tends to happen in cycles, related to menstrual cycles or life changes. Many people dealing with it have to manage recurring severe breakouts.
Common Symptoms of Hormonal Acne
Spotting symptoms early can lead to better treatment. Key signs are:
- Deep cystic spots that hurt and feel tender
- Outbreaks often happening around the time of menstrual periods
- Long-lasting nodular acne causing scars
- Acne mainly on the lower face and jawline
- Too much facial hair or unusual menstrual cycles can also happen due to high androgen levels
Hormonal acne can greatly affect a person’s confidence and skin health. Therefore, understanding its causes and signs is crucial for the right treatment.

| Characteristic | Details |
|---|---|
| Common Age Group | Typically starts in teenage years and can continue into 30s and during menopause |
| Typical Locations | Lower face, jawline, and chin |
| Symptoms | Painful cystic pimples, recurring nodular acne, possible hormonal irregularities |
| Treatment Options | Topical treatments, anti-androgens like spironolactone, birth control pills |
Causes of Hormonal Acne
It’s vital to know what causes hormonal acne to manage it well. Changes in hormones often trigger acne, especially in people from 20 to 50 years old. These changes can make the skin produce more sebum, clogging pores and starting acne.
Hormonal Fluctuations
Women deal with hormonal acne more because of changes in their hormones. This happens during their menstrual cycle, pregnancy, and menopause. High levels of male hormones, like testosterone, can make the skin’s glands produce too much sebum. This leads to acne.
Health issues like polycystic ovary syndrome (PCOS) make it worse. They throw hormones off balance, causing ongoing acne problems.
Key Triggers for Hormonal Acne
Many things can make hormonal acne worse. Some main triggers are:
- Stress: Stress can lead to more hormones that make the skin oily.
- Poor Diet: Eating lots of sugar and processed foods can upset hormonal balance.
- Lack of Sleep: Not getting enough sleep can mess with your hormones and cause acne.
- Oily Skin Products: Heavy makeup can block pores and make acne worse.
- Certain Medications: Some medicines, like those for testosterone, birth control, or steroids, can affect acne.
Improving your lifestyle can help with acne. Eating well, getting active, and managing stress are key.
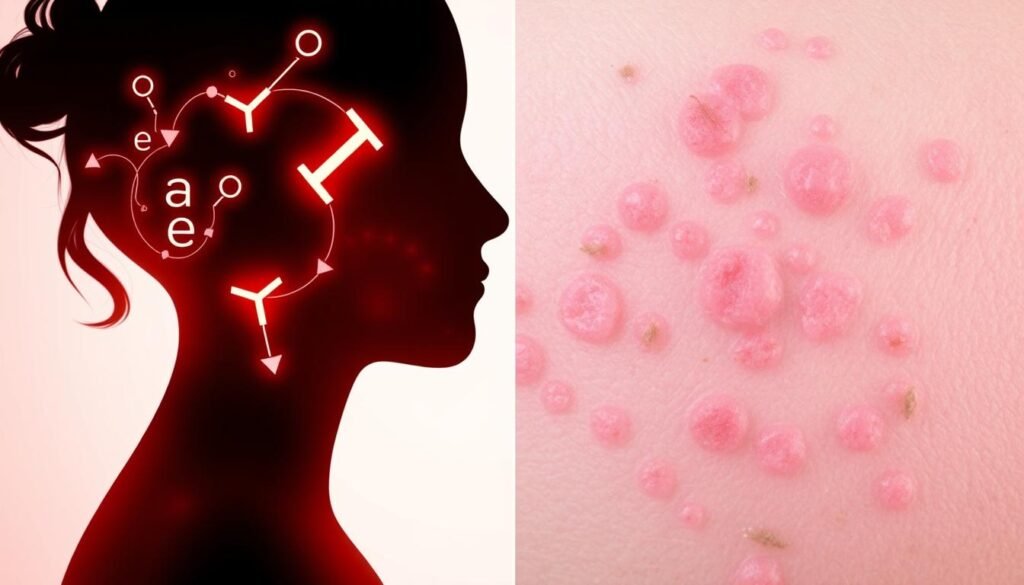
Fungal Acne vs Hormonal Acne: Key Differences
It’s vital to know the differences between fungal and hormonal acne. Spotting their unique acne appearance and symptoms helps tailor your treatment. This part will cover their looks, signs, causes, and what sparks them.
Appearance and Symptoms Comparison
Fungal and hormonal acne look and feel different. Fungal acne shows up as tiny, similar, itchy spots on the chest, back, and face. They often follow a pattern, setting them apart from other acne. On the other hand, hormonal acne appears as large, painful pimples. They mostly occur on the lower face, like the jaw and chin. Knowing these acne appearance differences is key to the right treatment.
Causes and Triggers Comparison
The reasons behind fungal and hormonal acne are not the same. Fungal acne comes from too much yeast on our skin. It gets worse with hot weather, heavy sweating, and using oily skincare. On the other side, hormonal acne is due to hormone level changes. This can happen with your period, pregnancy, menopause, or with PCOS. Spotting these acne triggers is essential for managing acne.
| Feature | Fungal Acne | Hormonal Acne |
|---|---|---|
| Type | Yeast Overgrowth | Hormonal Fluctuations |
| Common Symptoms | Small, uniform, itchy bumps | Deep cystic pimples |
| Typical Locations | Chest, back, face | Lower face, jawline, chin |
| Key Triggers | Hot weather, sweating, oily skincare products | Menstrual cycle, pregnancy, menopause |
Diagnosing Fungal Acne
To treat fungal acne right, it’s key to diagnose it correctly. Dermatologists use special ways to spot it and tell it apart from other acne. Looking closely at the skin helps find clear signs of it.
Visual Inspection by Dermatologists
A dermatologist first looks closely at the skin examination. They search for certain itchy bumps that are close together and look like under-the-skin pimples. They notice several things:
- Size uniformity of lesions
- Location of outbreaks, often on the chin, forehead, and upper back
- Itchiness of the bumps
This dermatologist insight helps tell fungal acne from hormonal acne, which looks different. If usual acne treatments don’t work but antifungal ones do, this suggests fungal acne.
Microscopic Examination Techniques
Sometimes, a closer fungal acne testing is needed. This means looking at affected skin samples under a microscope. Using swabs and skin scrapes helps find yeast detection. Spotting Malassezia yeast confirms fungal acne. This careful method makes sure patients get the best treatment.
If you face ongoing skin problems, get help from a pro. Spotting signs early could mean faster and easier treatment of fungal acne. Learn more on this webpage.
Diagnosing Hormonal Acne
To diagnose hormonal acne, a thorough review of the patient’s history is needed. Doctors look closely at the patient’s menstrual cycles and any issues like polycystic ovarian syndrome (PCOS). These might affect acne. This patient history helps find the triggers and create a fitting treatment plan. Checking symptoms is key. It shows the type and how bad the hormonal imbalances are.
Patient History Considerations
Detailed patient history helps doctors see what might cause acne. They look at changes in hormone levels, surroundings, and stress levels. Knowing these helps doctors suggest the right treatments and see how well they work over time.
Methods for Hormone Level Testing
For hormonal acne, testing hormone levels is important. Blood tests are usually used. They give important information about hormone imbalances. These laboratory assessments help make treatment plans that meet each patient’s needs. This detailed approach is vital for clear skin.
For more insights into the differences between fungal acne and hormonal acne, click here