About 85% of people between 12 to 24 years old get acne at some point. It’s mostly seen in teens but can continue into adult years, especially in women due to hormone changes. Knowing how bacterial infections cause acne is key to treating it. This is because acne can cause a lot of emotional stress and social worries.
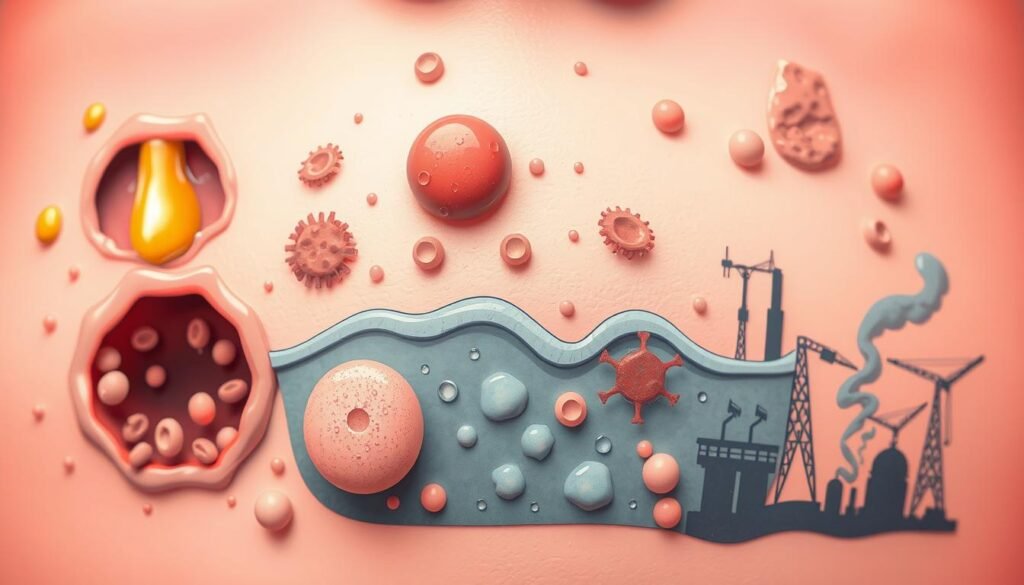
Acne starts when hair follicles get blocked with too much oil and dead skin. This creates a perfect spot for bacteria to grow. The cycle of oiliness and infection can make skin inflammation worse. It’s important to understand what causes acne and how to treat it. Overactive oil glands, hormone changes, and immune responses to bacteria play big roles. This article will look into these causes and show how to fight bacterial infections to keep skin clear and healthy.
Key Takeaways
- 85% of people aged 12 to 24 experience acne at some point.
- Acne can affect individuals of all ages, particularly women before menstruation.
- Excess oil production, clogged hair follicles, bacteria, and inflammation are the four main causes of acne.
- Types of acne include non-inflammatory (like blackheads) and inflammatory (including cysts).
- Effective treatments may involve topical and oral medications, light therapy, and dermatological procedures.
- Understanding the specific causes can help in managing and preventing acne outbreaks.
Understanding Acne: Overview and Types
Everyone gets acne at least once. It’s a common skin issue, especially during the teen years. This acne overview divides types of acne into two main groups. We have non-inflammatory acne, like whiteheads and blackheads. Then, there’s inflammatory acne, which includes papules, pustules, nodules, and cysts.
Teens usually start facing acne from 10 to 13 years old. But, 20% of adults battle with it too. Boys often have it worse than girls. But girls can deal with mild to moderate acne well into adulthood. You’ll mostly find these blemishes on the face. Yet, they can appear on the neck, back, and arms too.
Knowing the difference between non-inflammatory and inflammatory acne is key for treatment. The non-inflammatory kind is easier to manage with a good skincare routine. But, inflammatory acne needs quick action to avoid scars. For a deeper look into treating acne, check out this guide.
| Type of Acne | Description | Treatment Options |
|---|---|---|
| Whiteheads | Closed clogged pores that appear as small, white bumps. | Topical retinoids, exfoliation. |
| Blackheads | Open clogged pores that oxidize and darken. | Salicylic acid, benzoyl peroxide. |
| Papules | Small, inflamed bumps without pus. | Topical treatments, steroids. |
| Pustules | Similar to papules but filled with pus. | Oral antibiotics, topical treatments. |
| Nodules | Large, solid lumps beneath the skin. | Prescription medications, isotretinoin. |
| Cysts | Large, painful, pus-filled lesions. | Severe treatments, dermatological procedures. |
What Causes Acne? Factors Contributing to Outbreaks
Acne is influenced by many factors. A key cause is too much oil from sebaceous glands. This can happen when hormones change, like during puberty. These changes make the glands more active, leading to more sebum. This oil can block pores, which helps bacteria grow and inflammation start.
Changes in hormones, like those during menstruation or pregnancy, can also make acne worse. These changes can cause the sebaceous glands to act up. This is often why adults, especially women, get acne. It’s called adult-onset acne.
- Family history can increase acne risks.
- Certain meds, like steroids, can cause breakouts.
- High glycemic foods can also make acne worse.
- Environmental factors, like smoking, can affect adult acne.
It’s a myth that poor hygiene causes acne. The root causes are under the skin. It’s best to avoid harsh treatments, like popping pimples. It’s good to know that acne can’t spread from person to person.
So, acne comes from things like too much oil, hormone changes, genes, certain meds, diet, and the environment. Knowing these can help find the right treatment. It helps to focus on what specifically triggers your acne.
Role of Bacteria in Acne Development
Bacteria, especially Propionibacterium acnes, are key in acne growth. This specific bacterium lives in the oily parts of your skin. It’s usually harmless. But when pores are blocked, it multiplies fast, causing pimples.
This bacteria is deeply tied to acne. It not only fuels inflammation but also might make acne worse by producing harmful substances. About 10% of people worldwide suffer from acne due to it. Those with severe acne often have stronger reactions to this bacteria.
Eating lots of fats and dairy can also affect your skin. Such foods raise insulin, boosting acne bacteria growth and making acne more severe. If acne doesn’t get better with antibiotics, it might be due to more bacteria.
Knowing about skin bacteria is essential for acne care. Acne sufferers have different skin bacteria than those without acne. This affects how severe the acne is. In conclusion, Propionibacterium acnes plays a big role in causing acne, not just standing by.
Bacterial Infection in Acne: Symptoms and Identification
Bacterial infections are key in how acne develops and feels. It’s key to know the symptoms of acne for right treatment. This knowledge can show if it’s basic acne or a serious infection needing a doctor.
Common Acne Symptoms
Acne can show up in many ways. You may see:
- Red, inflamed sores on the face, back, and shoulders
- Pus-filled pustules that cause discomfort and make you feel self-conscious
- Blackheads and whiteheads from clogged pores
These symptoms of acne can really affect how you feel about yourself. This is especially true for young people dealing with this common issue.
How to Identify Infected Pimples
Infected pimples are worse than regular acne. You might notice:
- More redness around the pimple
- Swelling that spreads out from the pimple
- A warm feeling when you touch it, showing inflammation and infection
Knowing these signs of bacterial infection is key for getting the right help. Mild infections might get better with warm compresses and creams from the store. If the infection is bad or doesn’t go away, you might need to see a doctor for medicines like antibiotics.

| Symptom | Typical Acne | Infected Pimple |
|---|---|---|
| Redness | Minimal | Increased |
| Swelling | Minor | Significant |
| Warmth | No | Yes |
| Pain | Low | Higher |
Overactive Sebaceous Glands and Their Impact on Acne
Sebaceous glands getting too active play a big part in acne by making too much sebum. This grease, mostly on your face and scalp, leads to bacteria growth when pores get blocked with excess oil production. Understanding this shows why controlling sebum is key to handling acne.
How Sebum Production Fuels Bacterial Growth
Overactive glands make sebum levels shoot up. This extra sebum is a perfect place for bacteria to grow, leading to pimples. Research shows changing sebum’s makeup can make this worse. So, managing acne means focusing on effective treatments that keep sebum in check and fight the bacteria.
Consequences of Excess Oil Production
Too much oil makes bacteria grow and causes inflammation and redness. This can make acne worse and lead to scars. People with acne should try to control their sebum. Eating right and a good skincare routine can lower oil and ease acne.
Inflammation and Immune Response in Acne
The immune response in acne is very important in how the condition develops and worsens. When harmful bacteria invade clogged pores, the body fights back. This brings white blood cells to the site. As a result, we see red and swollen spots on the skin. These can hurt and make people feel upset.
Every type of acne shows some inflammation. Different skin immune cells take part in this battle. Among them are Langerhans cells, macrophages, and others. T and B cells also join in, making the immune reaction even more complex. People with severe acne have more antibodies against the acne bacteria than those with clear skin.
To treat acne well, we must focus on calming the inflammation. Using treatments that reduce inflammation and fight bacteria can make a big difference. For example, creams like adapalene and medicines such as dapsone are very effective. They help with various acne spots.
The way the immune system responds and causes inflammation greatly affects acne’s severity. Understanding these processes helps in creating better treatments. This means better results for those struggling. For more details on acne’s immune responses, click here.
Effective Treatments for Bacterial Infection in Acne
Bacterial infections can make acne worse and last longer. Luckily, there are many treatments available today. They include topical treatments and oral medications. Knowing about these options helps people choose the best care for their skin.
Topical Treatments and Their Efficacy
Topical treatments work by killing bacteria on the skin and reducing inflammation. Some common options are:
- Benzoyl Peroxide: This ingredient is great at fighting Propionibacterium acnes, a key acne bacterium.
- Salicylic Acid: It helps remove dead skin and clears pores, reducing pimples with regular use.
- Tea Tree Oil: Tea tree oil can improve acne in just 12 weeks.
- Niacinamide: It controls oil and lowers inflammation, helping with mild acne.
Oral Medications: When Are They Necessary?
For tougher acne cases, doctors might suggest oral medications. These include:
- Antibiotics for Acne: Tetracycline-class antibiotics are common, and a new antibiotic, sarecycline, is used for severe acne.
- Oral Contraceptives: These pills, which have estrogen and progestin, can control hormones that cause acne.
- Zinc Supplementation: Zinc can make antibiotics more effective against acne.
It’s key to balance topical and oral treatments for the best acne management. If you have severe acne, it’s best to see a dermatologist. They can suggest the right treatment plan for you.
| Treatment Type | Examples | Primary Benefits |
|---|---|---|
| Topical Treatments | Benzoyl Peroxide, Salicylic Acid, Tea Tree Oil | Reduces bacteria, exfoliates skin, and decreases inflammation |
| Oral Medications | Tetracycline-class antibiotics, Sarecycline, Oral contraceptives | Targets severe acne, regulates hormones, enhances effectiveness of other treatments |
Key Dermatological Treatments for Persistent Acne
Dealing with persistent acne calls for a detailed approach with different skin treatments. When usual methods fail, advanced options are needed. Treatments like chemical peels remove dead skin, cutting down on breakouts. Light therapy is also popular, using specific light to lessen inflammation and bacteria.
Isotretinoin works well for serious inflammation and bacteria issues. About 85% of people see clear skin after one isotretinoin cycle. It’s great for tough acne types. Meanwhile, hormonal issues might lead women to use birth control pills or spironolactone. They help balance hormones and reduce oil on the skin.

It’s vital to customize acne treatment to fit the person. Starting with treatments like benzoyl peroxide and antibiotics can greatly lower inflammation. Using multiple treatments together tends to work better. Sites like Mayo Clinic have details on effective treatments.
To tackle persistent acne well, stick to your care plan and see a doctor regularly. It’s key to apply treatments correctly for clear skin. People react differently to treatments, so getting advice from a dermatologist is crucial.
Lots of resources explain acne and how to manage it more simply. Sites like Glow Up Faces clear up myths, helping patients get the facts. This empowers them to choose the best therapy for their acne.
Essential Skin Care Regimen for Acne-Prone Skin
For those with acne-prone skin, finding the right skin care routine is crucial. It can greatly decrease breakouts and improve your skin’s health. Starting with strategies to avoid pore blockages is key to keeping skin clean and smooth.
Best Practices for Pore-Clogging Prevention
Selecting products that don’t cause acne is critical. Choosing the right ingredients enhances your skin care routine:
- Use CeraVe’s Acne Foaming Cream Cleanser with 4% benzoyl peroxide to fight acne.
- Exfoliate regularly with products that have azelaic acid at 10% to eliminate bacteria and lighten the skin.
- Apply CeraVe’s PM Facial Moisturizing Lotion. It has ceramides, hyaluronic acid, and niacinamide to calm and moisten the skin.
Choosing Oil-Absorbing Products
If you have oily skin, using products that absorb oil is beneficial. Here are some top picks:
- CeraVe’s AM Facial Moisturizing Lotion with Sunscreen moisturizes and protects with SPF 30 from the sun’s harmful rays.
- The CeraVe Resurfacing Retinol Serum helps with healthy skin renewal and prevents acne.
Adhering to these suggestions in your skin care routine can visibly improve acne-prone skin. Being consistent with your regimen enhances your skin health. It also complements any acne treatments you might be using.
Conclusion
Understanding acne management is key to dealing with its physical and emotional sides. The bacteria, especially Propionibacterium acnes and Staphylococcus epidermidis, play a big part in bacterial infection in acne. Knowing the signs and using a complete treatment plan improves skin and boosts self-esteem.
A careful skincare routine, with topical and oral treatments, is a must for those facing this chronic issue. Keeping up with hygiene and fighting harmful bacteria over-colonization helps reduce inflammation. This approach helps get clear, healthy skin and better overall health.
Recent studies on gut bacteria and acne show the importance of new treatments, like probiotics and diet changes, for skin health. As we learn more about acne’s complex nature, a comprehensive care strategy is vital. It supports skin health and personal confidence.