Did you know nearly 85% of people get acne at some point? Comedonal acne is really common, especially for those with oily skin, from kids to young adults aged 12 to 24. It shows up as small, flesh-colored bumps mostly on the chin and forehead. In this piece, we’ll cover the causes, symptoms, and treatment ways to aim for clear skin and healthy skin.
It’s key to know the different acne causes for good acne treatment. Things like hormones and what you eat can play a part. Treatment options range from creams to natural cures and changing your lifestyle. Taking good care of your skin not only stops breakouts but also makes it look better. For deeper insights, check out Medical News Today or Glow Up Faces.
Key Takeaways
- Comedonal acne mainly hits teens and adults with oily skin.
- Hormones and food choices are common triggers.
- Topical treatments and lifestyle tweaks can fight it.
- Regular skincare reduces acne.
- Knowing about different comedones helps in treating them right.
- See a dermatologist for tough cases.
Understanding Comedonal Acne
Comedonal acne is a milder acne type, marked by non-inflammatory spots. It develops when hair follicles get blocked by too much oil and dead skin cells. This acne affects people of all ages, especially teens, with rates ranging from 35% to over 90%.
Several things lead to comedonal acne. These are using oil-based skin products, genetics, hormone changes, and stress. While adolescent boys often get acne, it’s more common in adult women. More people in cities report acne than those in rural areas. Knowing what affects acne is key to treating it.
Knowing the types of acne helps understand how to treat them. Blackheads form when sebum, bacteria, dead cells, and hormone changes mix. Treatments focus on products like retinoids, salicylic acid, and benzoyl peroxide. Items like the Bliss Clear Genius Acne Spot Treatment use salicylic acid to fight oil. Meanwhile, Neutrogena Stubborn Marks PM Treatment uses retinol to boost cell renewal and keep new spots away.
Grasping the nuances of comedonal acne aids in picking the right management approach. People with skin problems should find treatments that suit their skin type. Starting treatment early and sticking to a skincare routine helps achieve clearer skin and a better complexion.
What are Comedones?
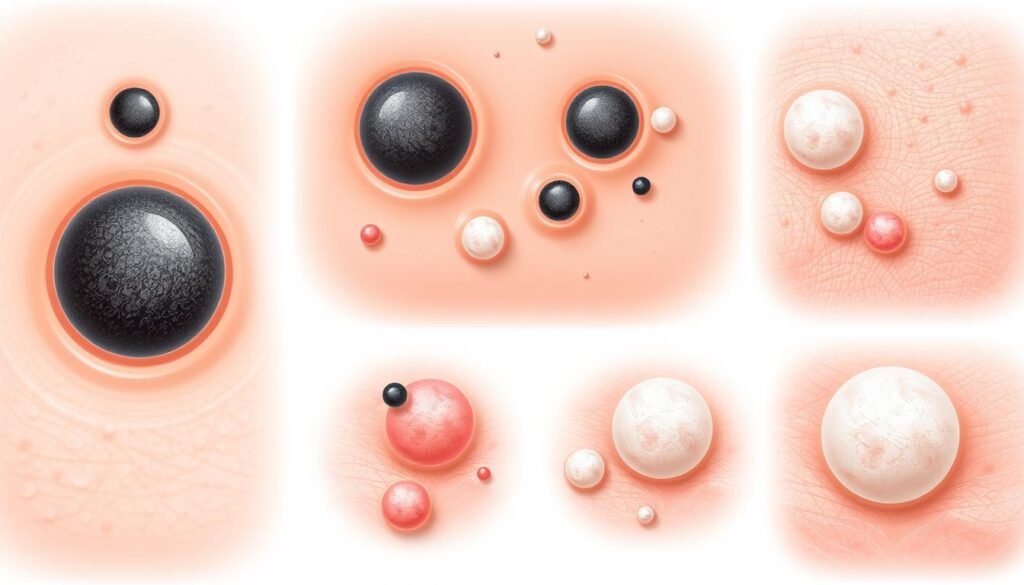
Comedones are small bumps that don’t cause inflammation. They mark the start of comedonal acne. These bumps can be open (blackheads) or closed (whiteheads). They form when hair follicles get clogged with too much oil and dead skin.
Comedones can show up on the face, back, neck, shoulders, and chest. Blackheads have a dark look because they’re open to air, causing the melanin to oxidize. Whiteheads, however, are flesh-colored and stay under the skin.
It’s important to know about the kinds of comedones for proper treatment. Microcomedones are tiny, almost unseen blemishes that can lead to bigger ones. On the other hand, macrocomedones are bigger, about 1 to 3 millimeters across. Comedonal acne isn’t just for teenagers; adults can get it, too.
The reasons people get comedonal acne differ. Genetics, oily skin, and hormone changes all play a role. While comedones aren’t red or swollen like other acne, not treating them can cause worse outbreaks.
| Type of Comedone | Description | Common Locations |
|---|---|---|
| Open Comedones (Blackheads) | Clogged pores that appear black due to oxidation. | Bridge of the nose, chin, shoulders, inside the ear, back. |
| Closed Comedones (Whiteheads) | Small, flesh-colored bumps, clogged with sebum and skin cells. | Forehead, chin, cheeks. |
| Microcomedones | Small, often invisible comedones. | Various locations; precursors to larger comedones. |
| Macrocomedones | Larger than average comedones, ranging from 1mm to 3mm. | Commonly found on the face and upper body. |
Comedonal Acne: Causes and Treatment
Understanding comedonal acne causes is key for good care. Many things lead to this issue, like clogged pores. These form open and closed comedones. Knowing why helps choose the best treatment for each skin type.
Common Causes of Comedonal Acne
Too much oil is a big cause of comedonal acne. Sebaceous glands that are too active make the skin oily. This traps dead skin, which lets comedones form. Hormones, especially during puberty and periods, also make more sebum.
Factors Contributing to Comedonal Acne
Many environmental factors can make comedonal acne worse. Air pollution and humidity can clog pores. This leads to more breakouts. It’s important to use non-comedogenic products. They don’t block pores and help lower acne risk.
The next table shows key factors linked with comedonal acne:
| Factor | Impact |
|---|---|
| Excess Oil Production | Leads to oily skin and clogged pores |
| Hormonal Changes | Increases sebum production during puberty and menstrual cycles |
| Environmental Factors | Pollution and humidity exacerbate acne conditions |
| Pore-Blocking Products | Can worsen acne by preventing skin from breathing |
For treatment, products like benzoyl peroxide and salicylic acid are helpful. They clear and calm the skin. If acne keeps up, seeing a dermatologist is smart. They might suggest chemical peels or retinoids. Knowing what causes comedonal acne helps pick the best care.
Types of Comedonal Acne
Comedonal acne comes in different types, each with its own features. Knowing these types helps pick the right treatment. It includes closed and open comedones, macrocomedones, and microcomedones. These are part of the comedonal acne family.
Closed Comedones (Whiteheads)
Closed comedones, or whiteheads, look like small bumps. They are either white or skin-colored. They form from oil and dead skin stuck in hair follicles. This oil gets trapped under the skin. Whiteheads usually show up around the eyes and mouth. They can get inflamed if bacteria infect the clogged pores.
Open Comedones (Blackheads)
Open comedones are known as blackheads because of their dark look. This dark color comes from oil that turns dark when it hits air. Blackheads often appear in oily areas like the nose, forehead, and chin. Spotting blackheads is key to managing them with the right skincare routine.
Macrocomedones and Microcomedones
Macrocomedones are big comedones that can stand out. They might look like whiteheads or blackheads but are bigger. On the other hand, microcomedones are tiny and hard to see. They are acne’s early stage and important in how acne starts. Even though they’re small, they play a big role in acne’s early development.
| Type of Comedonal Acne | Appearance | Common Locations |
|---|---|---|
| Closed Comedones | Small white or flesh-colored bumps | Face (around eyes and mouth) |
| Open Comedones | Darkened spots due to oxidized oil | Nose, forehead, chin |
| Macrocomedones | Larger, often inflamed bumps | Varies, commonly on the face |
| Microcomedones | Microscopic, not always visible | Any area prone to acne |
Symptoms of Comedonal Acne
It’s crucial to know the symptoms of comedonal acne for right treatment. This acne is different from other types, especially inflammatory ones. By knowing what makes it unique, we can find the best way to manage it.
Identifying Comedonal Acne
The symptoms of comedonal acne are usually small, smooth bumps. They aren’t red or swollen. You might see:
- Closed comedones (whiteheads) look like skin-colored or white bumps.
- Open comedones (blackheads) appear dark because of the air touching the debris inside the pore.
- Microcomedones are too small to see without magnification.
- Macrocomedones are bigger bumps that are easy to notice on the skin.
Knowing these types helps us spot comedonal acne and get the correct treatment.
Differences from Inflammatory Acne
It’s key to understand how comedonal acne isn’t like inflammatory acne for choosing treatments. Inflammatory acne often shows as:
- Red, painful bumps called papules and pustules.
- Deep, scarring nodules or cysts.
- It has more redness and swelling than comedonal acne.
Comedonal acne is less harsh and mainly on the surface, unlike inflammatory acne. This insight guides us to the right way to treat it, from store-bought products to expert advice.
Skincare Routine for Preventing Comedonal Acne
Having a regular skincare routine is key to stopping comedonal acne. It’s important to clean your skin well and pick the right products. By choosing a plan that fits your skin type, you can keep your skin clear and reduce acne.
Effective Cleansing Practices
Washing your face twice a day is crucial for fighting comedonal acne. Use gentle cleansers to get rid of excess oil and dirt. This keeps your skin’s moisture safe. Choose cleansers with salicylic acid or glycolic acid. They remove dead skin and unclog pores. Cleaning your face often keeps it acne-free and glowing.
Choosing Non-Comedogenic Products
Picking non-comedogenic items is essential for avoiding comedonal acne. These products don’t block pores, which helps people who easily get breakouts. Use oil-free moisturizers, makeup, and sunscreens to keep your skincare routine working. Avoid products with heavy oils or waxes as they can worsen acne. Adding non-comedogenic items to your daily care can greatly improve your skin’s health.

Topical Treatments for Comedonal Acne
There are many topical treatments for comedonal acne. They range from over-the-counter products to prescription medications. Using them consistently is key to getting good results.
Over-the-Counter Options
For starters, over-the-counter acne treatments are available. They have active ingredients aimed at comedonal lesions. Some popular choices include:
- Salicylic acid: It exfoliates the skin to prevent clogged pores.
- Benzoyl peroxide: It fights acne-causing bacteria with its antibacterial properties.
- Adapalene (Differin): A retinoid that promotes cell turnover to prevent breakouts.
- Glycolic acid: This alpha hydroxy acid sheds the skin’s surface layer.
Prescription Medications
When over-the-counter options don’t work, dermatologists may suggest stronger prescriptions. These might include:
- Retinoids: These are great for comedonal acne as they speed up skin renewal. Tretinoin and adapalene are common.
- Oral contraceptives: Women might use these to balance hormones that cause acne.
- Spironolactone: This can reduce androgens, leading to less oil production.
- Isotretinoin (Accutane): This is for severe acne cases that don’t improve with other treatments.
When starting a treatment plan, patience is vital. It often takes months to see big changes. A mix of topical treatments and lifestyle changes can offer the best way to manage comedonal acne.
| Treatment Type | Active Ingredient | Usage | Effectiveness |
|---|---|---|---|
| Over-the-Counter | Salicylic Acid | Apply directly to affected area | Effective for mild cases |
| Over-the-Counter | Benzoyl Peroxide | Apply after cleansing | Reduces bacteria and inflammation |
| Prescription | Tretinoin | Apply at night | Promotes skin turnover |
| Prescription | Isotretinoin | Oral medication | Severe cases resistant to others |
Natural Remedies and Lifestyle Changes
Using natural remedies and changing your lifestyle can help control comedonal acne. Eating better, exercising, and taking care of your skin are key. These actions lead to healthier skin and better overall health.
Dietary Modifications
What you eat plays a big part in fighting acne. Eating less dairy, fat, and sugar can help reduce breakouts. Eating more foods rich in antioxidants and drinking plenty of water improves your skin. Also, applying clay masks with jojoba oil can majorly improve acne after regular use for six weeks. Making these diet changes can lay a solid groundwork for battling acne.
Incorporating Exercise
Exercise is good for both your fitness and your skin. It boosts blood flow, helping clear out toxins, and can lower stress. Lower stress means fewer acne outbreaks caused by hormonal imbalances. Running, swimming, and yoga are great for your skin and acne control.
Skincare Habits to Adopt
Healthy skincare routines boost the power of natural remedies. Important practices are:
- Regularly cleaning the skin to remove oil and dirt.
- Choosing products that don’t block pores.
- Using treatments like tea tree oil to fight acne with its antimicrobial effects.
Aloe vera also helps soothe the skin, especially when used with ultrasound treatments to lessen skin problems. Adding these natural products to your daily skincare routine can help a lot. For more details on how acne develops, check out this article.
In-Office Treatments for Stubborn Comedones
If you’re dealing with stubborn comedonal acne, professional help can make a big difference. In-office treatments target the problem effectively, often better than home solutions. This part talks about the various professional procedures that help fight tough comedones.
Extraction Procedures
Extraction is a common way doctors get rid of comedones. It’s really good for removing blackheads and whiteheads. By cleaning out the pores deeply. Doctors use special tools and know how to do it with little pain. They also work to prevent scars. Getting extractions regularly can help your skin stay clear. It’s especially good for those who often have breakouts.
Microdermabrasion and Cryotherapy
Microdermabrasion is a deep exfoliation method. It uses fine crystals or a diamond-tip wand to take off dead skin and open pores. This makes your skin’s texture and look better. It’s a strong way to fight comedonal acne. Cryotherapy puts extreme cold on specific spots. It lowers swelling and helps heal. Both these treatments show real results in clinics.
When to See a Dermatologist
Knowing when to see a dermatologist for acne problems is crucial. This is especially true if regular treatments don’t work. Having persistent acne, like big, sore pimples or scars, means it’s time to get help. Look for signs that it’s time for an Acne Treatment Consultation.
If your skincare isn’t working after a few weeks, a professional might help you heal faster. This is important for those struggling with acne.
Acne Treatment Consultations help dermatologists understand your skin better. They suggest treatments that fit you, such as adapalene, azelaic acid, benzoyl peroxide, and salicylic acid. Benzoyl peroxide works well but start with a small amount to avoid irritation.
Acne treatments take time to work. You may see improvements in 4 to 8 weeks. Clearer skin can happen after 16 weeks. If you see dark spots after acne, called post-inflammatory hyperpigmentation (PIH), see a dermatologist to avoid worse issues.
Closed comedones can turn into big pimples if not treated. Hormonal changes and certain products can cause them. It’s important to watch how your skin reacts. Remember, treatments vary because everyone’s skin is different.

If over-the-counter options aren’t working for your acne, it’s time to see a dermatologist. Acting early can help control and prevent breakouts in the future.
Long-Term Management and Prevention Strategies
For long-lasting results against comedonal acne, a focus on Long-Term Management and Prevention Strategies is key. Such dedication greatly enhances the likelihood of achieving and keeping Clear Skin. It’s crucial to have a strong skincare routine, prioritizing both regularity and the quality of products.
Customizing your regimen based on skin type is important. This could involve:
- Using non-comedogenic moisturizers to avoid clogging pores
- Incorporating over-the-counter treatments like salicylic acid or benzoyl peroxide
- Practicing regular cleansing to eliminate excess oil and debris
- Avoiding heavy makeup or ensuring proper removal after use
A balanced diet plays a big role in achieving clear skin. Adjusting what you eat can work wonders. It’s smart to eat fewer high-glycemic foods, cut down on sugar, and limit dairy intake. Making these changes can help prevent breakouts and boost overall skin health.
Keeping an eye on your skin’s changes is vital for managing comedonal acne. Regular check-ins with dermatologists offer insights into your skin’s health and help tweak treatment plans as needed. Being up-to-date with the latest best practices and treatments is crucial for tackling skin issues confidently. Here’s a summary of key strategies:
| Strategy | Description |
|---|---|
| Regular Cleansing | Wash face twice daily using gentle, non-irritating cleansers. |
| Use of Non-Comedogenic Products | Opt for skincare and makeup products that do not clog pores. |
| Balanced Diet | Focus on low-glycemic foods while limiting dairy and sugars. |
| Routine Dermatological Visits | Schedule regular check-ups to adjust strategies and products. |
| Sun Protection | Limit sun exposure and use oil-free sunscreen daily. |
Adopting these treatment and lifestyle changes helps in the extensive management of acne. Through prevention and a proactive stance, clearer skin can be a realistic target.
Conclusion
Grasping the details of comedonal acne is key for handling and treating it right. Knowing the causes, like hormonal shifts and environmental influences, helps people work towards better skin. A strong skin care plan that involves soft cleansing and safe products is critical for stopping more outbreaks.
Adding topical solutions, from over-the-counter or from doctors, can greatly aid in managing closed pores. Ingredients such as salicylic acid and retinoids are good for dealing with existing spots and blocking new ones. Also, making changes in your diet and exercise routine can boost your skin’s overall health.
Being active and well-informed about treating comedonal acne is essential in fighting its impact. Sticking to your skin care routine and getting expert advice when needed can lead to clearer skin and more confidence.